Tendons: Why They Hurt and How To Treat Them. Hint: It's Not Rest
Why tendons hurt... and how to avoid injuring them.
Summary
Tendinopathy is the leading cause of tendon pain, a broad term encompassing failed adaptation, structural changes, and associated pain.
Causes include abrupt load increase, repetitive cycles, compression + tension, intrinsic tissue limitations, and failed repair responses.
Rest alone is never sufficient. Tendons need load to remodel and regain capacity.
A smart rehab progression moves from isometrics to strength loading. Tendons eventually require heavy loads to heal.
Prevention is as important as treatment.
Tendon-related pain is exceptionally common. I see more people in the office for tendon pain than for any other issue. Most of these “injuries” are self-inflicted, either from doing too little or too much.
And although I’m biased… this is a very good, in-depth overview of why our tendons hurt and how to treat them. I can guarantee you that most (including doctors) do not understand these principles.
Tendons adapt to load. They require a load to be healthy. But how that load is applied matters.
When someone says, “My tendon hurts,” it helps to pause and think: why?
Many people reflexively say “inflammation” and “tendinitis,” but tendinitis is actually rare in adults.
Tendinopathy is a far more common cause.
Let me explain.
Why Tendons Hurt — Tendinitis vs. Tendinopathy
“Tendinitis” suggests inflammation: swelling, redness, infiltration by immune cells… a classic “itis.” That model works in cases of acute overload or acute tears. However, chronic tendon pain rarely exhibits a strong inflammatory cell presence under the microscope.
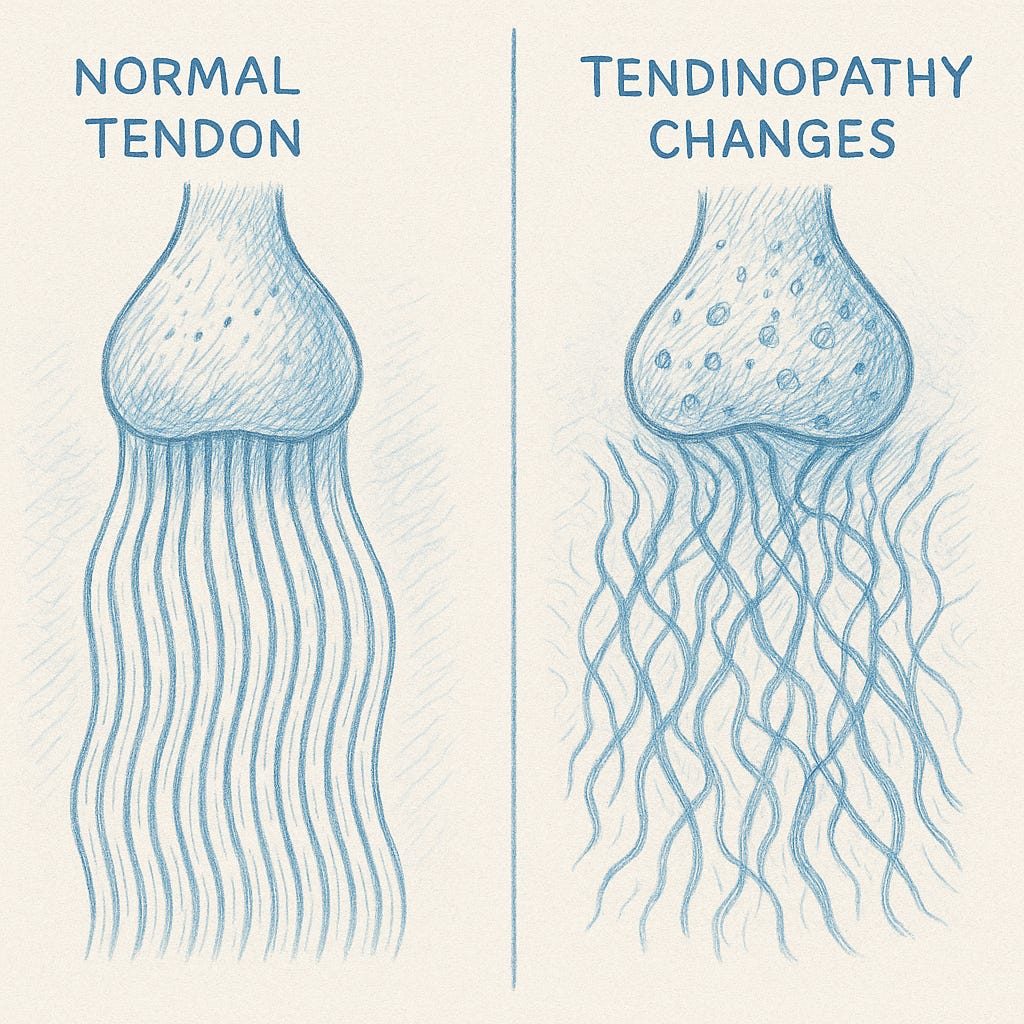
Instead, it tends to show disorganized collagen near its attachment to bone, microruptures, increased ground substance (which I’ll explain), excessive vascular and neural (including pain) ingrowth, and “degenerative” changes. I hate using the term degeneration… but it’s relevant.
Now… many of you have probably had MRIs that have shown evidence of tendinopathy. Most people with tendinopathy have no pain. But some people with tendinopathy have terrible pain.
We’re not always sure why that happens. However, towards the end of this article, I delve into the common training errors. (or lack of training) that can lead to painful tendons.
When we biopsy or examine tendons in chronic painful states, traditional inflammatory markers (neutrophils, massive inflammatory cell infiltrates) are often absent or minimal.
That doesn’t mean that inflammatory mediators (cytokines, signaling molecules) aren’t involved, but the concept of a purely “inflamed tendon” fails to capture what’s going on.
Thus, the preferred term is tendinopathy. This captures the broader idea: pain, dysfunction, structural changes, failed adaptation, partial degeneration.
It does not assume that inflammation is the sole culprit, but rather allows for variable contributions from multiple processes.
Tendinopathy means the tendon is not adapting well to load. Alternatively, it may be failing due to the absence of a load. In tendinopathy, the tendon is struggling. It may have microdamage, disordered collagen, and zones that are less capable of repair.
Pain and structure don’t always align: sometimes a tendon “looks bad” but causes no symptoms, while sometimes pain is present despite mild changes. So we must treat the person, not just the MRI or ultrasound images.
For Members, I dive into the details of why common tendinopathies, such as tennis elbow, achilles tendinopathy, patella tendinopathy, and rotator cuff tendinopathy, occur, and how to manage them.
And, no, the treatment is not simply rest. It’s never rest. Furthermore, since prevention is the most effective strategy, the final section provides robust guidelines to follow to minimize the risk of tendon issues.
Tendons require load to heal and retain capacity.
Keep reading with a 7-day free trial
Subscribe to Built to Move, Born to Heal: Notes on Midlife Fitness to keep reading this post and get 7 days of free access to the full post archives.