No, Exercise Doesn't Cause or Worsen Osteoarthritis. Keep Going, If You Can.
A lot of people with osteoarthritis (OA) have been told the same thing: “Slow down. Protect your joints. Don’t push it.” It sounds cautious, even responsible. But it’s wrong, and it’s one of the main reasons people with OA lose function, gain weight, slip into frailty, and develop the downstream problems that shorten their lives.
Exercise does not cause osteoarthritis, and it does not make osteoarthritis progress faster. The research consistently shows the opposite. Movement protects joints. It improves symptoms. It improves quality of life. It preserves healthspan.
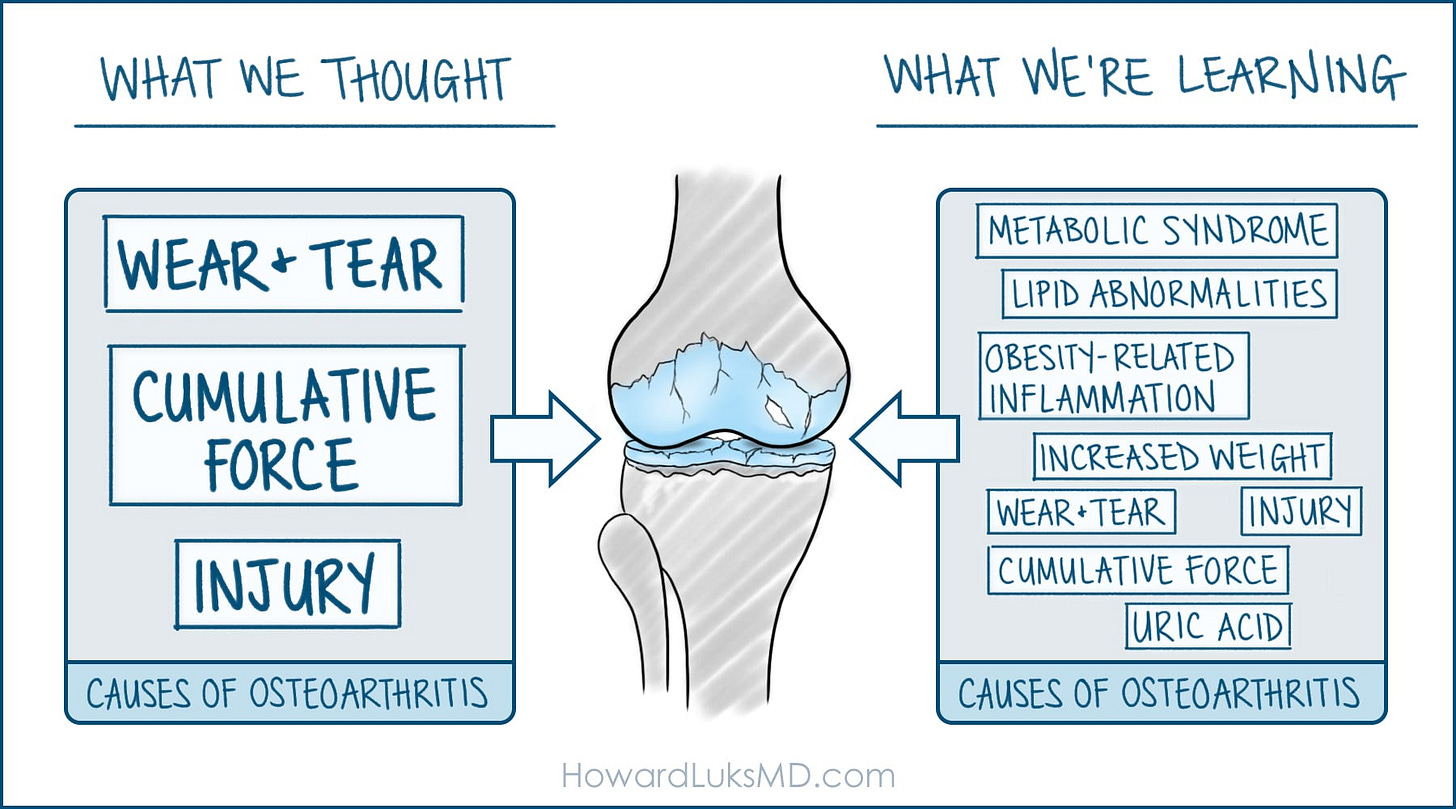
OA is far more often the result of biological and metabolic factors than mechanical ones. The idea that joints “wear out” with use has never aligned with the science. What actually drives OA in many people is a metabolic environment marked by inflammation, insulin resistance, and disrupted cartilage homeostasis—not movement. And the consequences of avoiding activity—thinking you’re preserving your joints—are far worse than the arthritis itself. Genetics, as well as prior injury or surgery, will affect risk, too. But…
It’s time to retire the fear-based narrative around osteoarthritis and exercise.
OA Is Often a Metabolic Disease, Not a Wear-and-Tear Process
Osteoarthritis strongly overlaps with metabolic syndrome. Insulin resistance, visceral adiposity, dyslipidemia, and elevated inflammatory cytokines all play direct roles in altering cartilage biology. Adipokines, such as leptin, and cytokines, such as IL-6 and TNF-alpha, interfere with cartilage turnover and accelerate degenerative changes. This metabolic fingerprint predicts OA progression far better than the amount of physical activity someone performs.
The most obvious sign that OA is not a load-driven disease is its higher prevalence in non-weight-bearing joints. Hand and wrist OA are far more common in patients with obesity. If OA were purely due to weight, this would not be the case. These joints are not exposed to the repetitive impact blamed for OA in the hips, knees, or spine. But they respond to systemic inflammation and metabolic stress.
Osteoarthritis is not a passive erosion of cartilage caused by using the joint. It is an active biological process influenced by metabolic dysfunction.
The Myth That Load Causes OA Misses the Biology Entirely
The belief that exercise or joint loading causes osteoarthritis comes from a purely mechanical view of human joints. Cartilage, tendons, ligaments, and subchondral bone are not static materials. They are living tissues designed to respond to load. Intermittent compression improves nutrient diffusion into cartilage, keeps synovial fluid circulating, strengthens bone, and maintains collagen alignment in ligaments and tendons.
Remove the load, and these tissues weaken. Apply it correctly, and they remodel and become more resilient.
The simplistic “wear and tear” model ignores the metabolic, inflammatory, and endocrine factors that have far greater influence on joint health than how much someone walks or lifts. The biology is complex. The myth is simple. And it has misled millions of people into avoiding the very thing that could help them most.
Exercise Improves OA, Symptoms, and Function
Large randomized trials consistently show that exercise improves pain, mobility, and strength without accelerating structural degeneration, even in people with moderate or severe OA. Strength training improves neuromuscular control and joint mechanics. Aerobic training reduces systemic inflammation and improves insulin sensitivity, lowering the metabolic burden that drives OA progression. People who exercise function better, hurt less, and preserve more of their independence.
Movement is treatment. Avoidance is harm.
The Real Risk Is Inactivity
People with osteoarthritis tend to move less, not because movement is dangerous, but because they’ve been told it is, or their intuition tells them that it is. Granted, their degree of pain has a role as well. But if their pain is that bad, then it’s time to see a surgeon. Otherwise, an awful course spiraling downward occurs, less activity, worsening health, worsening pain, even less activity, a narrowing world, depression, loneliness, sickness, and worse.
A drop in activity triggers a predictable chain of events: deconditioning, weight gain, worsening insulin resistance, declining cardiovascular function, muscle loss, bone loss, fragility, and reduced physical capacity.
This downward slope—not joint damage—is what leads to disability and higher mortality over time. Many of us have seen this in loved ones; it’s an awful problem.
OA is not fatal, per se. But the sedentary lifestyle that often follows an OA diagnosis can be.
What Actually Protects People With OA
Movement protects joint structures and the tissues around them. Walking, cycling, resistance training, balance work, and neuromuscular training stimulate cartilage nutrition, support joints with stronger muscles, improve coordination, reduce inflammation, and restore metabolic health. These are the interventions that slow OA biology and improve quality of life. In the book I published here on Wednesdays from the summer through just a few weeks ago, we reviewed many treatment options to alter the trajectory of decline that often accompanies a diagnosis of osteoarthritis. Furthermore, most Orthopedic Surgeons will tell you that those of you who maintain your strength and abilities will keep your natural joints the longest.
Avoiding movement protects nothing.
What’s Holding You Back?
Exercise doesn’t cause osteoarthritis. It doesn’t worsen it. It protects the joint, the body, the heart, the brain, and the lifespan. Inactivity, fear, and avoidance are the real threats. Exercise is also one of the best treatments for arthritic joints. Yes, some of you will have too much pain to do certain activities. Yes, you might need to alter some of your exercises or skip them entirely. But if you get to the point where you can’t do anything because of pain, we need to have a chat in my office.
If you were told to “save your joints” by moving less, you were given bad advice that’s not backed by science and 30 years of experience. Pulling back from activity does not protect anything, but it does accelerate decline.
Move. Train. Walk. Cycle. Lift. Your joints—and your entire physiology—depend on it.
References
Courties A, Sellam J. Osteoarthritis and the metabolic syndrome: emerging relationships. Joint Bone Spine.
Berenbaum F, Eymard F, Houard X. Osteoarthritis, inflammation and obesity. Curr Opin Rheumatol.
Messier SP et al. Exercise and osteoarthritis outcomes. Arthritis Rheumatol.
Bennell KL, Hinman RS. Exercise as first-line therapy for OA. BMJ.
Veronese N et al. Osteoarthritis and mortality: a systematic review. Semin Arthritis Rheum.
Nilsen T et al. Physical inactivity mediates the association between OA and mortality. Osteoarthritis Cartilage.
Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet.
Roos EM, Arden NK. Mechanical load and joint health. Osteoarthritis Cartilage.
Felson DT et al. Physical activity and cartilage health. Ann Intern Med.
Bricca A et al. Effectiveness of exercise for osteoarthritis: systematic review. Br J Sports Med.



Good article.
Good to read an MD that is conversant in physical fitness.
I say this because you tend to agree with Pavel Tsatsouline.
From ‘Power to the People’:
“ As for the bit of advice about not locking out your joints, it is all hogwash. Your joints were meant to lock and support load. In fact, if you do not subject them to stress, you will never be really strong!”
Fantastic information and well-presented. Thanks for this article.