Can We Decrease Our Risk of Developing Severe Osteoarthritis?
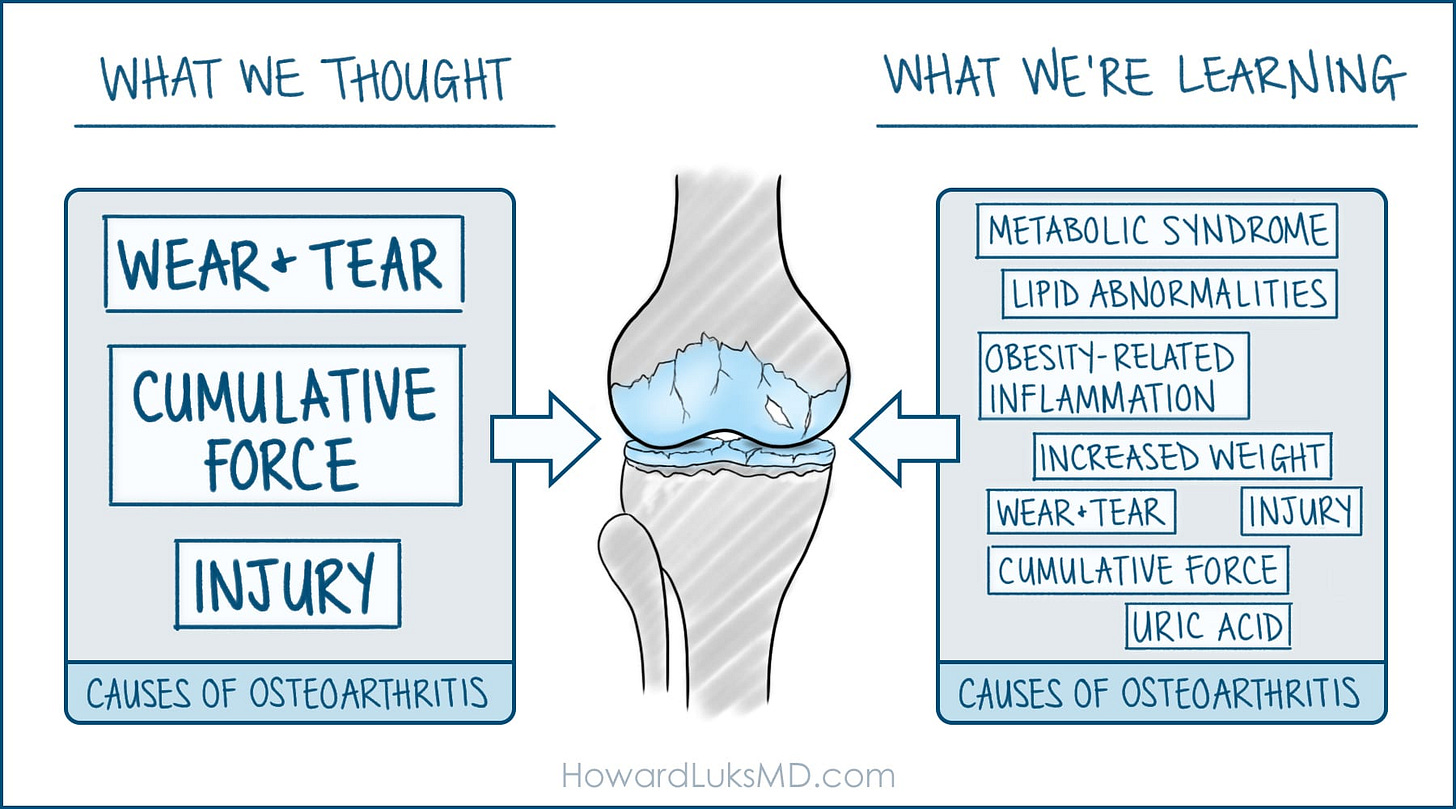
For decades, we thought osteoarthritis (OA) was simple. You used your joints. They wore out. Mechanical wear and tear. Cumulative force over time → Injury.
That model made sense. It was clean. It was easy to explain. But it was incomplete.
We’re learning that osteoarthritis is far more complex than we realized. It’s not just a mechanical breakdown. It’s a biological process driven by systemic factors that most people - and many doctors - never connect to joint health.
Metabolic syndrome. Lipid abnormalities. Fatty liver. Visceral fat. Obesity-related inflammation. Uric acid elevation.
These aren’t separate issues that happen to coexist with arthritis. They’re drivers of the disease process itself.
Your metabolic health affects your joints. Insulin resistance creates systemic inflammation. Elevated lipids contribute to cartilage degradation. Uric acid doesn’t just cause gout - it’s been linked to osteoarthritis development and progression. Elevated glucose levels (and A1c) cause your collagen to cross-link and impair its function. The chronic low-grade inflammation that comes with poor metabolic health doesn’t stay confined to your bloodstream. It affects your cartilage, your joint fluid, and your entire joint environment. The joint environment goes from being nourishing and reparative to hostile and degenerative.
This changes everything about how we should approach arthritis prevention and treatment. At least it should…
Yes, injury still matters. Prior surgery and cumulative force still matter. Wear and tear play a role... at levels far greater than most of us will ever achieve. But they’re not the whole story. Maybe not even the biggest part of the story.
When I see a patient with knee pain and early arthritis, I’m not just looking at their X-rays anymore. I’m looking at their fasting insulin. Their lipid panel. Their uric acid. Their inflammatory markers. Their body composition.
Because addressing their metabolic health might do more for their joints than anything I can inject or operate on.
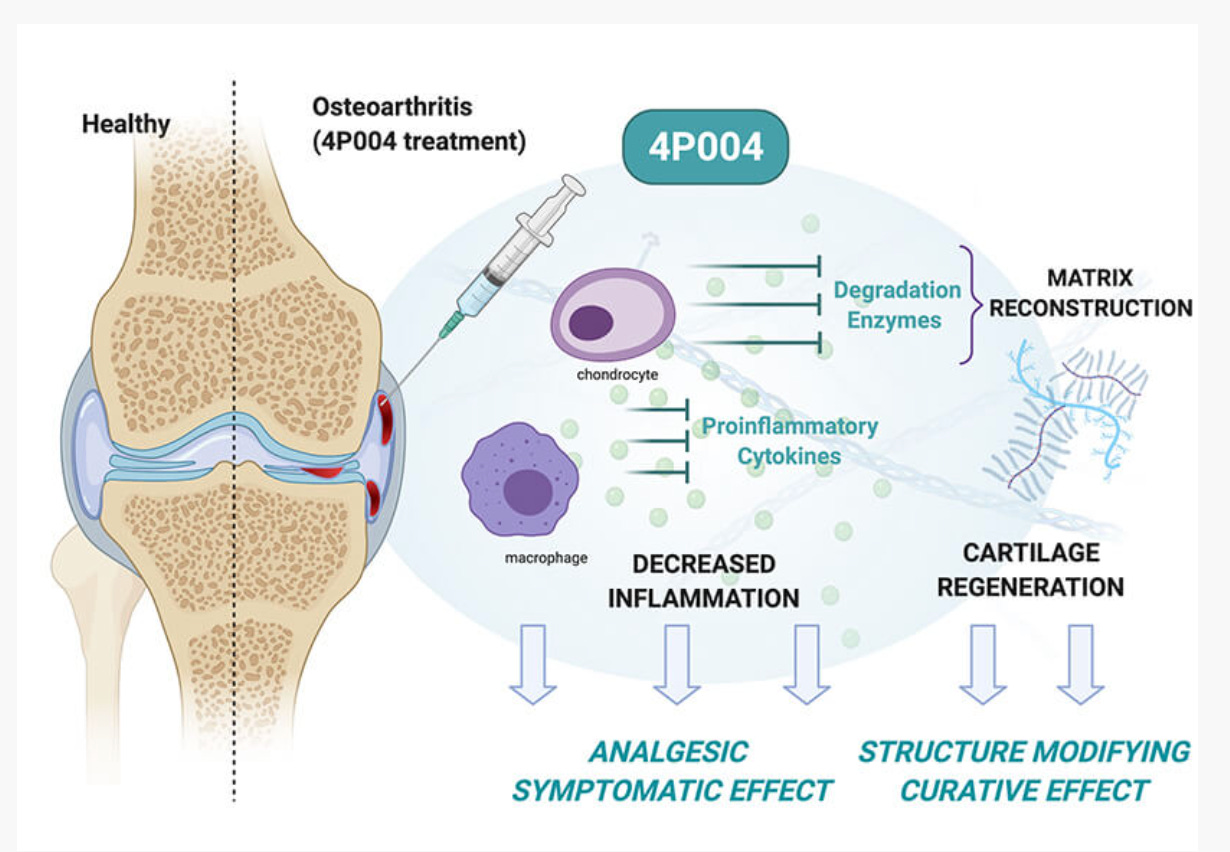
This is why the runner with good metabolic health can log thousands of miles without developing arthritis, while the sedentary person with metabolic dysfunction develops it anyway. Yes, there’s often more to it… But this model holds. And it’s also why one of the first actual disease-modifying drugs for osteoarthritis will be an injectable GLP1. Because the mechanical load isn’t the determining factor. The biological environment is
.
To decrease the risk of developing OA, and decrease the rate of progression of OA, we need to fix your metabolic health - improve your insulin sensitivity, lower your systemic inflammation, normalize your lipids, manage your weight - and you’re not just reducing your risk of diabetes, dementia, and heart disease. You’re protecting your joints. You’re also not broken if it’s already started within some of your joints. Because you can influence the rate of progression. And aging remains the leading cause of osteoarthritis.
Osteoarthritis is almost inevitable... but you can influence when it starts to bother you and how quickly it progresses.
Stay strong- The stronger your legs, the longer you’ll keep your natural joints.
Stay active- walking is proven to be one of the best treatments for OA.
Fix your diet.
Fix your sleep
Measure what matters 2-3x/year: A1c, fasting insulin, lipids, homocysteine, uric acid, CRP, IL-6.
Address the abnormalities
Just walk, walk often throughout the day, occasionally with ferocious intent.
OA is not just “wear and tear.” It’s a disease process we can influence.
And that influence starts with metabolic health.
-Howard


Great article! I wish more orthopedic surgeons and physical therapists would address metabolic health and osteoarthritis and tendon/ligament issues. Thank you.
Fascinating article Howard thank you for sharing. I coach T2D clients in my fitness business and I’m amazed by how many think they can eat what they want once they’re on meds such as Metformin. they ignore their metabolic health completely